When I eventually came to, I was instinctively holding a tissue to the wound, not knowing where I was or how I got there. I tried to piece the events together to no avail. My wet matted hair and damp skin told me that I had been in the shower. The gaping wound on my forehead I could not explain. After making my way to the closest hospital, I was stitched up, and much to my reluctance, told to stay overnight. I would only find out what had happened to me later that evening when I awoke to find a disgruntled, overworked nurse peering into my eyes.
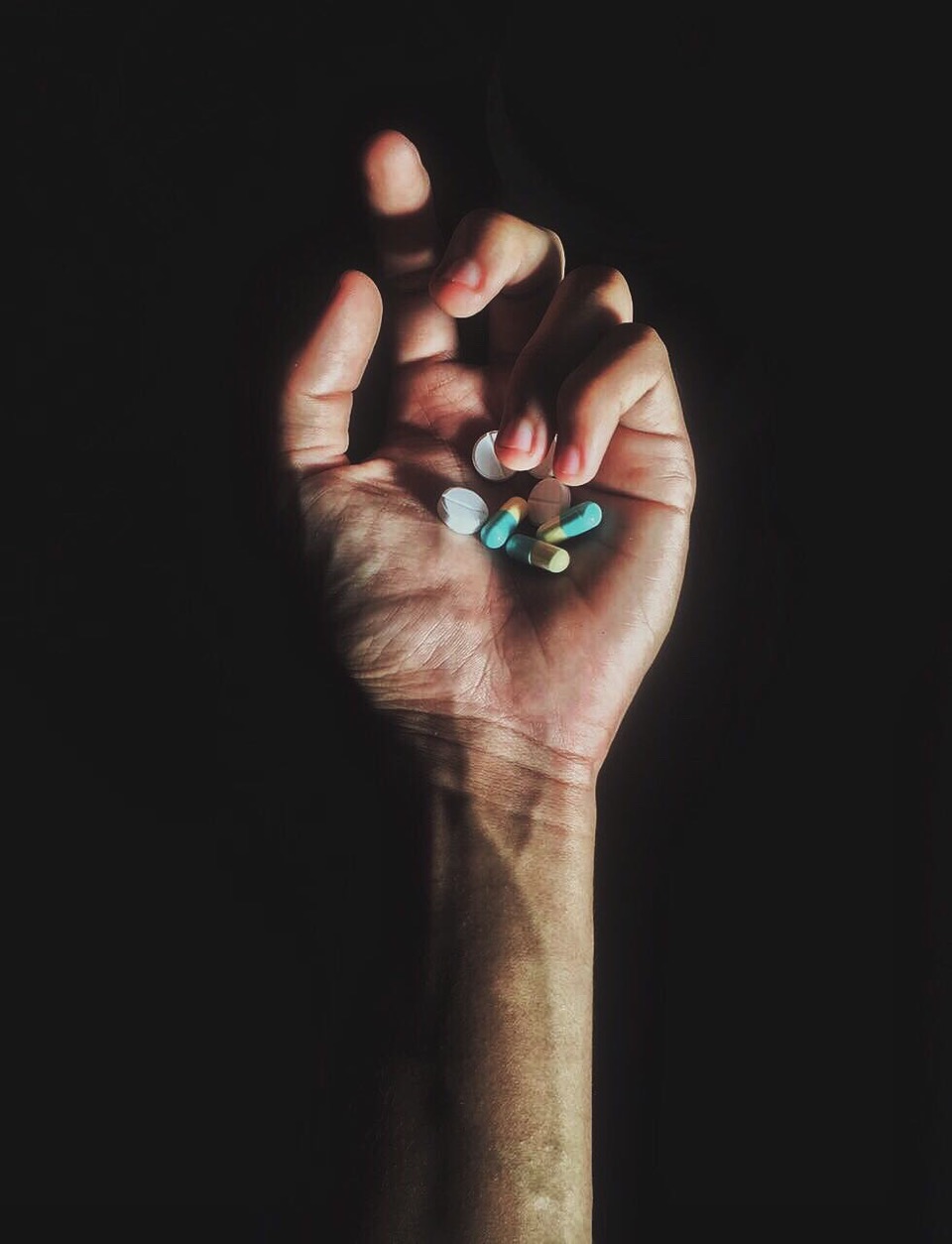
She informed me that I had had two seizures whilst in her unit and would need to be transferred to the neurology department. “Was I on any medication?”, she probed. I told her that yes, I took Xanax for anxiety, generally daily but I had missed a dose. She shrugged and rolled her eyes, “Oh that’s what caused it,” she sighed, “you’re in withdrawal.” She seemed relieved to have finally figured me out.
It is somewhat strange that I have such clarity in recalling this moment, given that my head had recently been given a severe shaking for the third time that day. On the other hand, I just received the news that turned my life upside down. I, as she so nonchalantly pointed out, was an addict. ‘Benzodiazepine dependent’.
It was while living in Los Angeles several years ago, during the peak of American overmedication in 2008, that I first came across Xanax. Alprazolam (the pharmaceutical name for Xanax) is in a family of ‘mild’ tranquilisers called benzodiazepines, and is commonly used to treat anxiety and insomnia.
As regular in the medicine cabinets of my West Coast friends as virgin coconut oil, Xanax seemed like a Californian rite of passage.
I had been yearning for an anxiety ‘cure’ for much of my life. My stern childhood doctor prescribed exercise and therapy. Like many others who turn to pharmaceutical alternatives, I wanted fast results and I wanted them now.
After visiting the physician of a friend and describing my struggles with anxiety, I walked away with a 1mg per day script for Xanax for the next month. Initially I found the results extraordinary. The nervous tic in my right eye disappeared. I managed to make it through the day without blushing or sweating. I slept better than I had in years. For a chronically nervous person, it was a wonder drug. I felt like an upgraded version of myself.
Within a couple of weeks, however, the positive effects had somewhat plateaued. Upon reporting this to the doctor, my dose was doubled. I was prescribed 2mg Xanax for the better part of two years. Unbeknownst to me, it was a rather hefty amount, for anyone.
In hindsight, I should have been more vigilant about what I was putting into my body. The normalization of prescription medication can have a placating effect. I didn’t think to question the dangers of something so readily available. Coupled with my desperation to rid myself of debilitating anxiety, I fell into the trap of quick-fix society.
Had I done my research, I would have found that benzodiazepines like Xanax are highly addictive, and should only be prescribed in the short term. Perhaps I placed too much trust and confidence in medical professionals to correctly prescribe and verbally inform their patients of associated risks. Perhaps I was also unwilling to put in the hard yards required to be mentally at ease.
After a while the symptoms of my nervousness began to resurface with an additional influx. I hadn’t noticed it at the time, but I had begun to change. My mind seemed to be clouded in an endless fog, and I had become sullen and withdrawn. Friends told me that I had been slurring my words, and simple motor skills eluded me. Nevertheless, I continued with my routine medication, occasionally doubling up on particularly stressful days. It was after neglecting to fill my script during the holiday season that I found myself bewildered, naked and bleeding on the bathroom floor. Little did I know, the nervous systems kicks into overdrive during benzodiazepine withdrawal, and seizures are a common result.
At the hospital, the doctors informed me that I would need to go through a detox process if I wanted to properly come off my medication. I was stunned. Until recently, I had never heard the words ‘addiction’ and ‘withdrawal’ used in association with Xanax. Now that was all I was hearing. I agreed, afraid of another lapse in consciousness. No one prepared me for what was to come next.
I was switched to Valium (Diazepam), which is a longer acting less potent benzodiazepine. Within a week they had weaned me off and sent me home. I should be feeling better, they said. Free from dependence. That was not the case. A couple of days later, the real anguish began. Constant tremors and muscle spasms set in. I was struck by blurred vision, memory loss, sudden dyslexia, cramps and general high voltage in my nervous system. I felt like a stranger in my own body. It was as if there was an inexperienced puppeteer in my brain pulling the wrong strings. If I thought my anxiety was bad before, this was an entirely new level. I would have done anything to return to old, pre-Xanax self.
I couldn’t understand why I had been so ill-informed. For a medication that is so often prescribed, no one seemed to be able to give me much information. It was in those harrowing days that I made the decision to go back on Xanax. Only this time, I was dangerously self medicating, supplementing my dose with scripts I obtained through doctor shopping. My thirst for this drug had amplified in withdrawal. I felt like the addict the nurse had described at the hospital. No longer unaware of the risks, I felt immense guilt and shame. I stumbled along this path for another few months before eventually returning home to Australia to get some help.
Initially, I didn’t have much luck here either. I encountered similar gaps in knowledge about benzodiazepine addiction and withdrawal as I had in America. After enrolling in a rehabilitation facility, I was placed on another rapid withdrawal scheme. It wasn’t long before I was flung into the same place of despair. The doctors grew weary of me, and were unmoved by my pleas for a slower reduction. To be fair, the staff at rehab clinics are busy and are used to patients attempting to bamboozle them. But benzodiazepine withdrawal is a strange beast.
My symptoms had still not subsided in a month, but I was told that this was simply not possible. The drug was long out of my system, and I should no longer be reacting to it. I began to question my own sanity and wondered if it was all in my head.
Three months after my withdrawal at the treatment centre, I found myself in familiar territory. Fed up with the continued pain of withdrawal and my inability to function, I took some Xanax that had been saved for emergency situations. Doctor shopping for benzodiazepines turned out to be just as easy in Australia as it had been stateside. In a couple of months, I was back where I started. I was distraught, thinking I would never be able to free myself from this cycle.
After again seeking help, I was fortunate enough to finally find a doctor who understood the unpredictable nature of benzodiazepine withdrawal. He advised me that long term benzodiazepine use can permanently alter neurotransmission and cause an early onset of dementia. Long term use is considered to be anything in excess of three months. He also explained the concept of protracted benzodiazepine withdrawal, a notion that users can be affected for many months or even years following withdrawal.
The more times a person attempts to withdraw, the more drawn out and gruelling the process becomes. The doctor recognised that as a long term user with several withdrawal attempts to my name, I was suffering from protracted benzodiazepine withdrawal syndrome. It was a relief to have found a medical professional that acknowledged my plight.
This time around, I was put on a slow-scale withdrawal system that took six months to complete. The doctor saw my level of commitment and treated me as an outpatient. After completion I suffered very minor symptoms, nothing like I had previously endured. Under his supervision I was able to return to some semblance of normality. My memory resurfaced, as did my cognition.
Twice weekly sessions with a psychologist and a course of cognitive behavioural therapy helped to ease the psychological symptoms of my withdrawal, and some of the deep seated reasons behind my anxiety. This is what was required all along. After taking these steps I have managed to remain benzodiazepine free for the last few years.
Although I do take responsibility for my own actions, I overwhelmingly believe that I would not have found myself in this predicament had there not been such a lax societal attitude to these very dangerous and addictive drugs. I feel exceedingly frustrated when I see casual references to Xanax and Valium on television, as if it’s the most natural thing in the world to pop one when you needed some chill out time.
Benzodiazepines are a class of drugs that are said to be more addictive than opiates, and should be treated as such. It is not just America that is being over-tranquilised. Last year around 10 million scripts were written for benzodiazepines in Australia. What people really should know, is that in the long term these pills can do much more harm than good. Ironically, prolonged benzodiazepine use can heighten anxiety and depression. They only work to suppress anxiety, not treat it. As I learned, the nervous energy just boils beneath the surface and reemerges twofold.
It is not only the ease of falling into benzodiazepine dependence that troubles me, but the lack of understanding about withdrawal. Rapid benzodiazepine withdrawal is very dangerous and can cause death. This is most likely due to seizures in unexpected places, such as what I experienced in my shower stall. You cannot die from opiate withdrawal, painful as it may be. What my struggles have taught me is that not everyone follows the same withdrawal trajectory. There is no one size fits all treatment. Patients needs should be assessed individually and in accordance with their pattern of use. Failure to provide adequate treatment only leads to further isolation, and often further benzodiazepine abuse and misuse.
Being addicted to anything is hard enough, let alone something that is misunderstood by many in the medical community and other addicts alike. It seems like doctors are happy to put patients on Valium or Xanax, but when it comes time to withdraw they are not interested. Often the only place for benzodiazepine dependant individuals to seek solace and information about their condition is through online forums started by fellow sufferers. Many don’t attend support groups such as Alcoholics Anonymous and Narcotics Anonymous, as they don’t feel like it is the right fit for them.
In the years since I’ve been Xanax free, I have come to accept that to some degree, I’ll always be a nervous person. What I have learned to do is not take anxiety so seriously and embrace it for what it is. It is freeing to no longer have that same sense of foreboding that followed me around for so long.
Although I have been in recovery for several years, I have a permanent reminder of that time in my life. The scar I wear through my left eyebrow is symbolic of my descent into unwitting addiction, and my ability to pull myself back out.
For assistance and information:
SMART Recovery Australia – an AA alternative focused on addictive behavioural patterns. Session are in small groups.
Reconnexion – A Melbourne based organisation that provides both online and group support to help recognise dependence and treat withdrawal.